Recent research has shed new light on the underlying mechanisms of long COVID (post-COVID syndrome or PCS), revealing a crucial link between persistent nasal inflammation and the lingering symptoms experienced by many individuals. A collaborative team of scientists from the Research Center Borstel, Leibniz Lung Center (FZB), Kiel University (CAU), the University of Lübeck (UzL), and the University Medical Center Schleswig-Holstein (UKSH), among others, have identified specific molecular drivers responsible for this inflammation.
Understanding Long COVID and the Research Challenge
Long COVID is a growing concern, affecting approximately 3–17% of people after a SARS-CoV-2 infection. Those affected grapple with a wide range of persistent and debilitating symptoms, and the exact causes of these prolonged effects remain largely elusive. This lack of understanding has hampered the development of effective treatments.
Novel Insights from Single-Cell Analysis
To address this challenge, the researchers employed advanced single-cell transcriptomics (scRNA-seq) combined with sophisticated cell biology models. This technique allowed them to examine the cellular and molecular processes occurring within nasal tissue at an unprecedented level of detail. The study utilized nasal biopsy samples from 25 patients participating in NAPKON, a nationwide post-COVID cohort, allowing for a representative sample of individuals experiencing long COVID.
Key Findings: TNFα and TGFβ Driving Persistent Inflammation
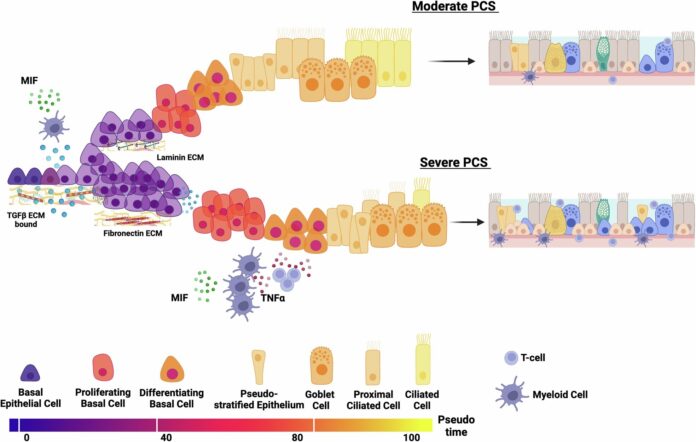
The researchers’ analysis uncovered significant alterations in the structure and function of the upper respiratory tract mucosa, even months after the initial SARS-CoV-2 infection – and in the absence of ongoing viral activity. They pinpointed two crucial “messenger substances” – TNFα and TGFβ – that are responsible for driving persistent inflammation in the nasal mucosa.
The Role of TNFα and TGFβ
These substances appear to disrupt the normal programming of cells within the mucosal tissue, hindering the regenerative processes necessary for healthy functioning. Specifically, researchers found that the combination of TNFα and TGFβ severely disrupts the regeneration of the ciliated epithelium, a vital layer of cells that clear debris and pathogens from the airways.
“Our data show that the combination of the two messenger substances, TNFα and TGFβ, severely disrupts the regeneration of the ciliated epithelium,” explains Dr. Karosham Reddy.
Implications for Symptoms and Susceptibility
This persistent inflammation prevents the airway mucosa from maintaining its protective function, potentially leading to prolonged respiratory symptoms and an increased susceptibility to infections—both common features of PCS. It’s important to understand that the inflammation is not maintained by the virus itself, but by these downstream messengers triggered by the initial infection.
Potential for Targeted Treatments
The findings, published in Nature Communications, offer a promising new avenue for treating long COVID. By identifying specific signaling pathways involved in PCS, researchers hope to develop therapies that can alleviate symptoms and potentially prevent long-term damage to the nasal mucosa.
“Our observations point to specific signaling pathways that appear to play a key role in PCS. These could be therapeutically targeted to alleviate symptoms and possibly prevent long-term damage to the nasal mucosa,” says lead author PD Dr. Fähnrich.
Looking Ahead: Broader Implications for Chronic Lung Diseases
Researchers believe these findings may also be relevant to other chronic lung diseases, opening up possibilities for future studies exploring shared underlying mechanisms and potential therapeutic approaches. This research significantly advances our understanding of the complex biological processes that contribute to long COVID, providing a critical foundation for developing effective treatments and improving the lives of those affected.